Renal Transplant Imaging: Essential Protocols for Donor and Recipient Assessment


- Introduction
- Imaging the Kidney Donor
- Ultrasound Evaluation
- CT Angiography of kidneys (CTA): The Gold Standard
- Findings in an Optimal Donor Candidate
- Role of MRA in Donor Imaging
- Imaging the Kidney Recipient
- Ultrasound (US) in Recipient Evaluation
- CT Angiography (CTA) of kidneys for Recipient Assessment
- Findings in a Suitable Recipient Candidate
- Donor-Recipient Matching and Imaging Confirmation
- Post-Transplant Imaging
- Ultrasound with Doppler: First-Line Modality
- CT/MRI for Complications
- Conclusion
- References
Introduction
Every year, thousands of kidney transplants depend on precise imaging for success. Renal transplant procedures require meticulous preoperative imaging to ensure the best outcomes for both donors and recipients. The ability to accurately assess renal vasculature, anatomical variations, and potential complications can significantly impact the success of the transplant and long-term graft function.
As of 2024, approximately 100,000 Americans remain on the kidney transplant waitlist, yet only 22,817 transplants were performed in 2020, with less than one-third from living donors. This disparity highlights the urgent need for efficient donor evaluation processes to maximize organ utilization.
Imaging plays a crucial role in assessing donor anatomy, evaluating recipient suitability, and aiding in surgical planning. Computed Tomography Angiography (CTA) kidney imaging is the gold standard for preoperative donor assessment, offering high-resolution imaging of renal vasculature and anatomy. In cases where iodinated contrast is contraindicated, Magnetic Resonance Angiography (MRA) serves as a viable alternative. A study across 32 countries revealed that 13% of transplant programs use both chest and abdominal CT scans for deceased donor evaluation, while 6% integrate these scans with chest radiography. These variations in imaging protocols emphasize the importance of tailored approaches to donor assessment and transplant success.
This article outlines the imaging modalities, protocols, and findings relevant to renal transplant ultrasound and radiology, emphasizing the technical aspects that radiologic technologists, sonographers, and radiologists must consider. We will first discuss renal transplant ultrasound for the kidney donor, followed by imaging techniques for the recipient, detailing essential protocols and key findings.

Imaging the Kidney Donor
A thorough evaluation of potential kidney donors is essential to confirm anatomical suitability, rule out underlying pathology, and minimize surgical risks. The primary imaging modalities used include ultrasound, computed tomography angiography (CTA), and magnetic resonance angiography (MRA).
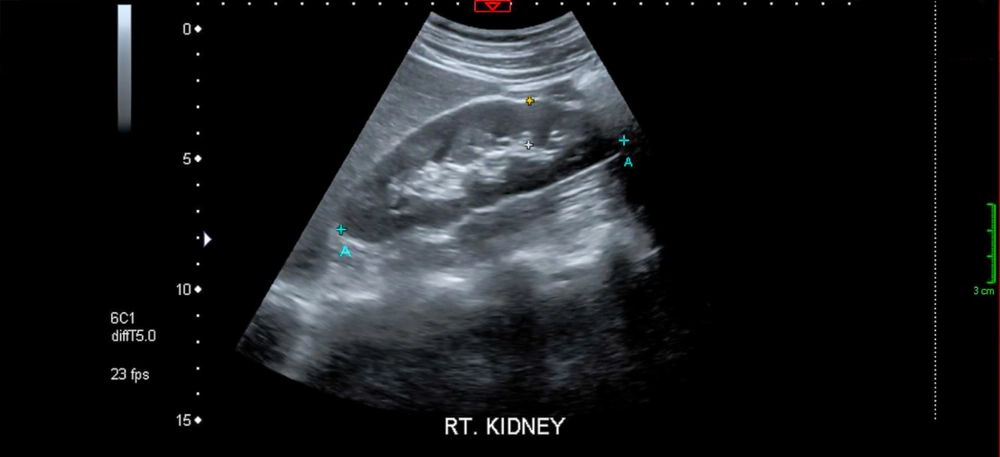
Ultrasound Evaluation
Renal transplant ultrasound is an essential first-line imaging modality for evaluating renal conditions, offering advantages such as accessibility, the absence of ionizing radiation, and the ability to provide real-time assessment of both renal anatomy and vascular flow. This non-invasive approach is typically used for initial screening to detect renal abnormalities, including cysts, tumors, or hydronephrosis. The technique often combines B-mode imaging, which provides detailed anatomical images of the kidneys, with renal transplant Doppler ultrasound protocol techniques to assess renal vasculature and perfusion.
Findings from a normal renal transplant ultrasound evaluation include a standard renal size and echotexture, the absence of significant masses or cystic disease, and symmetric blood flow to both kidneys, indicating healthy perfusion.
- Purpose: Initial screening to detect renal abnormalities such as cysts, tumors, or hydronephrosis.
- Technique: B-mode imaging combined with renal transplant Doppler ultrasound protocol for assessing renal vasculature.
- Findings: Normal renal size and echotexture, absence of significant masses or cystic disease, and symmetric perfusion.
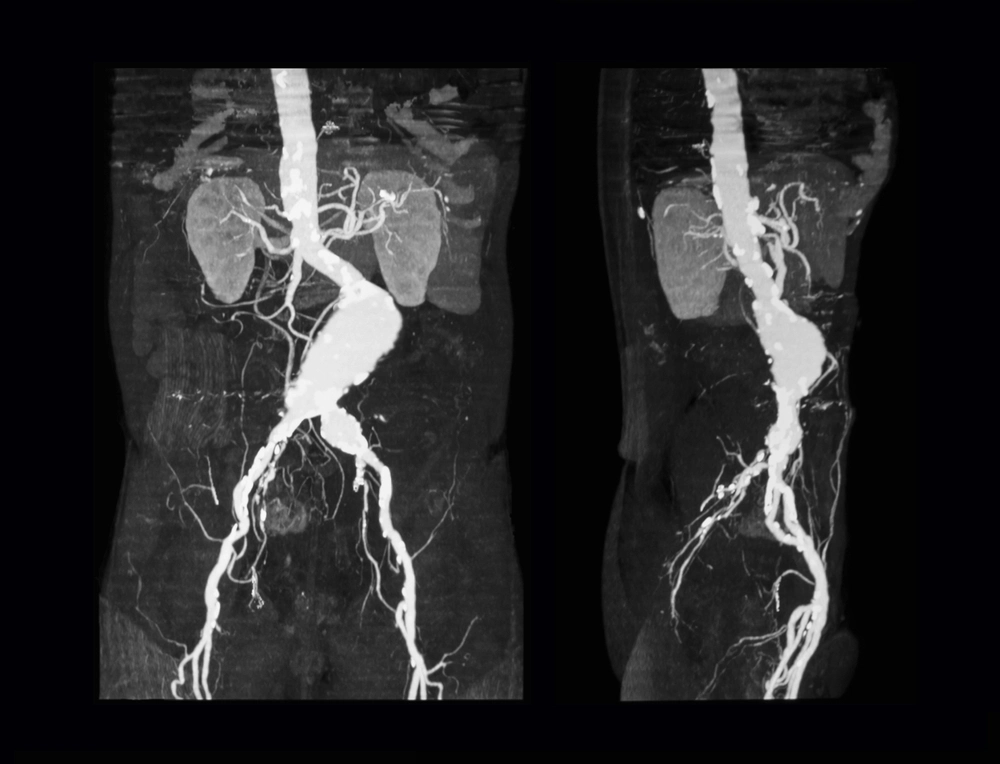
CT Angiography (CTA): The Gold Standard
CT angiography of the kidney provides high-resolution imaging of the renal vasculature, parenchymal anatomy, and collecting systems, making it a critical tool for surgical planning in kidney transplantation. The CT protocol for donor evaluation is performed in multiple phases to capture detailed information at each stage. The non-contrast phase evaluates the renal parenchyma and detects nephrolithiasis. The arterial phase, occurring 20-30 seconds post-contrast injection, maps the renal arterial anatomy and identifies accessory arteries. The venous phase, 50-60 seconds post-injection, assesses renal and systemic venous drainage, while the excretory phase, 5-10 minutes after injection, visualizes the ureters and potential anatomical variations. Key parameters for optimal imaging include a slice thickness of 0.5-1.25 mm for detailed vascular and parenchymal assessment, the administration of 100-150 mL of iodinated contrast at a high injection rate, and optional dual-energy CT for advanced tissue characterization and stone composition analysis. Given the global variability in imaging protocols, it is important to standardize CTA techniques to ensure consistency in donor evaluation
CT Protocol for Donor Evaluation
- Phases
- Non-contrast phase: Evaluates renal parenchyma and detects nephrolithiasis.
- Arterial phase (20-30 sec): Maps renal arterial anatomy, and detects accessory arteries.
- Venous phase (50-60 sec): Assesses renal and systemic venous drainage.
- Excretory phase (5-10 min): Visualizes ureters and potential anatomical variations.
- Key Parameters:
- Slice thickness: 0.5-1.25 mm for detailed vascular and parenchymal assessment.
- IV contrast: 100-150 mL of iodinated contrast administered at a high injection rate.
- Dual-energy CT: Optional for advanced tissue characterization and stone composition analysis.
Findings in an Optimal Donor Candidate
A comprehensive imaging evaluation helps determine whether a donor is suitable for a renal transplant. The following findings indicate an ideal donor candidate:
- Single renal artery and vein per kidney (though multiple vessels can be managed surgically)
- No renal pathology (e.g., masses, cysts >5 cm, significant scarring).
- Symmetric kidney size and function with good cortical-medullary differentiation.
- Absence of significant atherosclerosis or fibromuscular dysplasia in renal arteries.
For donors with iodinated contrast allergies or reduced renal function, MRA is a viable alternative for vascular mapping.
Role of MRA in Donor Imaging
Magnetic Resonance Angiography (MRA) serves as an alternative to Computed Tomography Angiography (CTA) in kidney donor evaluation, particularly in cases where iodinated contrast agents used in CTA pose a risk. MRA is preferably used for donors with iodine contrast allergies, pre-existing renal impairment, or concerns about radiation exposure. Unlike CTA, which relies on ionizing radiation and iodinated contrast, MRA utilizes gadolinium-based contrast agents, which have a lower risk of nephrotoxicity, making it a safer option for patients with reduced renal function. Additionally, non-contrast MRA techniques, such as time-of-flight (TOF) and phase-contrast imaging, can effectively map renal vasculature without contrast administration. However, MRA has limitations, including lower spatial resolution compared to CTA, longer acquisition times, and susceptibility to motion artifacts, which may hinder the precise visualization of small accessory renal arteries. While CTA remains the gold standard for preoperative planning due to its superior vascular detail and faster scan times, MRA provides a valuable alternative in select patient populations.
Comparison of CTA vs. MRA for Kidney Donor Imaging
| Feature | CTA (Computed Tomography Angiography) | MRA (Magnetic Resonance Angiography) |
|---|---|---|
| Contrast Agent | Iodinated contrast (nephrotoxic) | Gadolinium-based (lower nephrotoxicity) |
| Radiation Exposure | Yes (ionizing radiation) | No (radiation-free) |
| Resolution | High spatial resolution | Moderate spatial resolution |
| Imaging Speed | Fast (seconds) | Slower (minutes) |
| Best For | Standard evaluation, surgical planning | Patients with iodine contrast allergy or renal impairment |
| Limitations | Radiation exposure, nephrotoxicity risk | Motion artifacts, lower arterial resolution |
Imaging the Kidney Recipient
Pre-transplant imaging in recipients ensures the viability of transplant placement, evaluates vascular status, and detects potential complications.
Ultrasound in Recipient Evaluation
Ultrasound of kidney transplants plays a vital role in providing a baseline assessment of the native kidneys and bladder before transplantation. Doppler imaging is particularly important for evaluating the iliac vessels, ensuring their patency, and identifying any thrombus or stenosis that could impact the success of the transplant. Normal findings include adequate blood flow through the iliac artery and vein, with no evidence of significant stenosis or occlusion, confirming a suitable vascular environment for graft implantation.
- Purpose: Baseline assessment of native kidneys and bladder.
- Doppler Imaging: Evaluates iliac vessels for patency, thrombus, or stenosis.
- Findings: Normal iliac artery and vein flow, no evidence of significant stenosis or occlusio
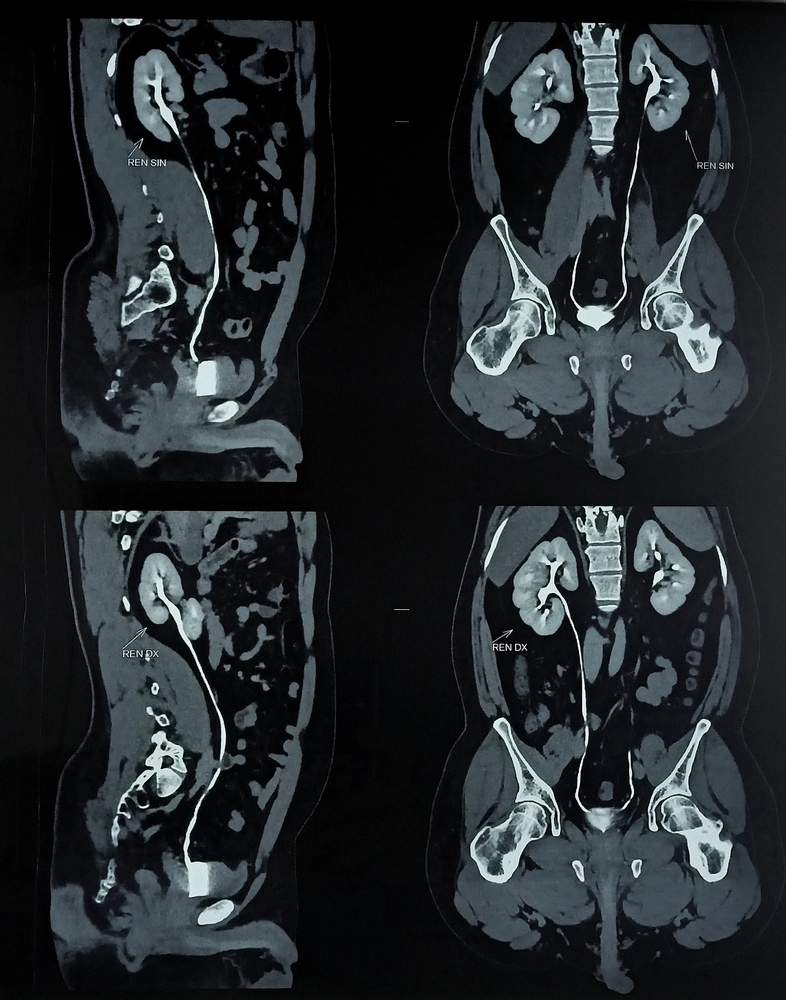
CT Angiography (CTA) for Recipient Assessment
CT angiography in kidney imaging is essential for assessing vascular anatomy and identifying potential complications that could impact transplantation. CTA is essential for assessing vascular anatomy and identifying potential complications that could impact transplantation. The protocol includes multiple phases to provide comprehensive imaging. The non-contrast phase detects vascular calcifications and atherosclerosis, which may influence surgical planning. The arterial phase evaluates iliac artery anatomy and detects stenosis, while the venous phase assesses iliac vein patency and the presence of thrombus. Key imaging parameters include a slice thickness of 0.5-1.25 mm for optimal vessel visualization, contrast volume similar to donor CTA with a focus on iliac vasculature, and 3D reconstruction to aid in planning vascular anastomosis, ensuring a successful transplant procedure.
CT Protocol for Recipient Evaluation
- Phases
- Non-contrast phase: Evaluates vascular calcifications and atherosclerosis.
- Arterial phase: Assesses iliac artery anatomy and stenosis.
- Venous phase: Evaluates iliac vein patency and possible thrombus.
- Key Parameters:
- Slice thickness: 0.5-1.25 mm for optimal vessel visualization.
- Contrast volume: Same as donor CTA with emphasis on iliac vasculature.
- 3D reconstruction: Provides surgical planning details for vascular anastomosis.
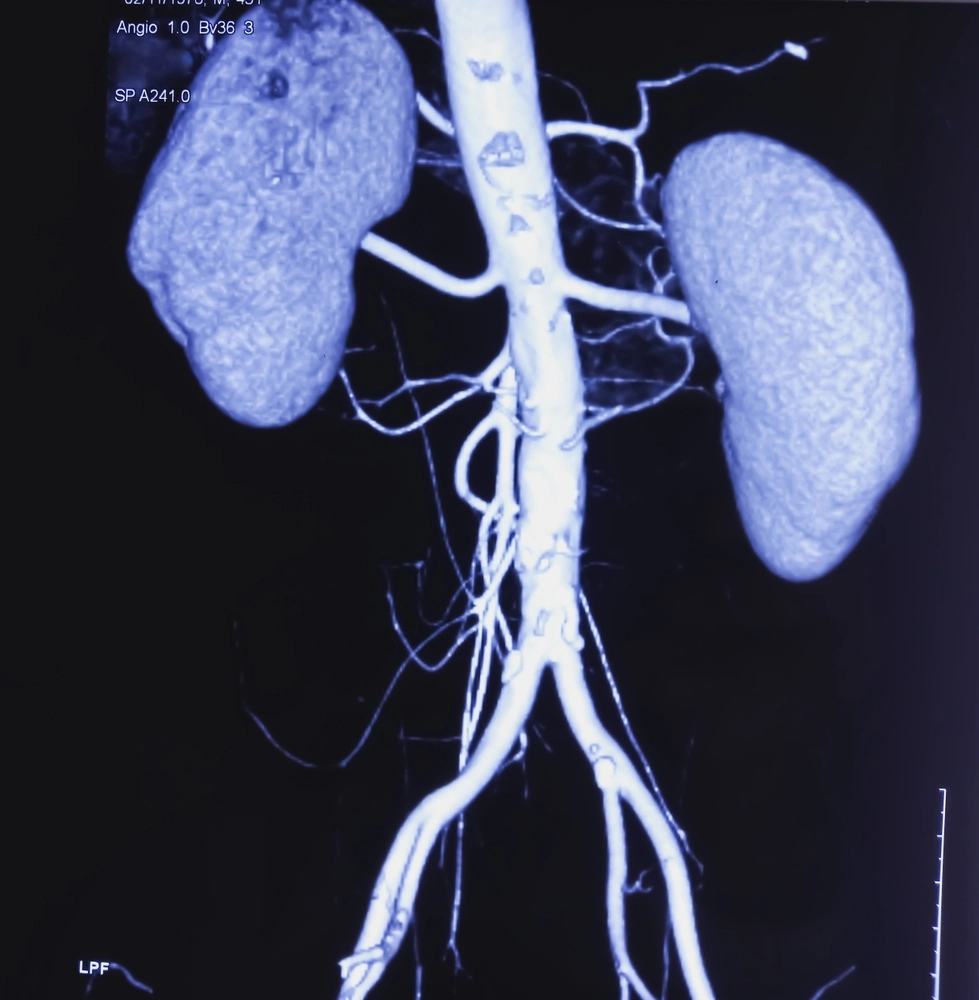
Findings in a Suitable Recipient Candidate
In a suitable renal transplant recipient, imaging findings should confirm optimal vascular and urinary conditions for a successful procedure. The iliac arteries and veins must be patent, without significant stenosis or calcification, ensuring proper blood flow to the transplanted kidney. Adequate bladder function and capacity are essential to accommodate urinary drainage from the graft. Additionally, there should be no evidence of significant systemic vascular disease that could compromise transplant viability or long-term graft function.
- Patent iliac arteries and veins without significant stenosis or calcification.
- Adequate bladder function and capacity to accommodate urinary drainage.
- No evidence of significant systemic vascular disease that could impact transplantation.
Donor-Recipient Matching and Imaging Confirmation
Successful kidney transplantation relies on multiple compatibility factors, including:
- Blood type compatibility (ABO matching).
- HLA (human leukocyte antigen) matching to reduce rejection risk.
- Negative crossmatch test to confirm no pre-existing donor-specific antibodies.
- Imaging confirmation ensures donor anatomy and recipient vascular integrity align for transplantation.
Imaging confirmation requires a thorough assessment of the donor and recipient’s vascular structures to ensure anatomical compatibility and optimize surgical planning. In the donor, CT or MR angiography is essential to map renal vasculature, confirming the number, course, and caliber of renal arteries and veins while ruling out vascular anomalies that could complicate nephrectomy. For the recipient, imaging focuses on evaluating iliac vessel patency, ensuring adequate arterial and venous flow to support the transplanted kidney. Additionally, cross-sectional imaging aids in identifying any potential obstructions, thrombi, or calcifications that could impact graft function. This comprehensive imaging approach minimizes surgical risks and enhances the likelihood of long-term transplant success.
Post-Transplant Imaging
After a renal transplant, imaging plays a crucial role in evaluating graft function, detecting early complications, and guiding clinical management. The success of a renal transplant depends on maintaining adequate blood flow, ensuring proper urinary drainage, and identifying any structural abnormalities that could compromise the graft. Imaging is particularly valuable in the immediate postoperative period to assess vascular integrity and perfusion, as well as in long-term follow-up to monitor for rejection, infection, or chronic allograft dysfunction. A multimodal imaging approach, incorporating ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), provides a comprehensive assessment, aiding in early intervention when complications arise. According to kidney.org, early detection of complications via imaging modalities significantly enhances long-term transplant success.
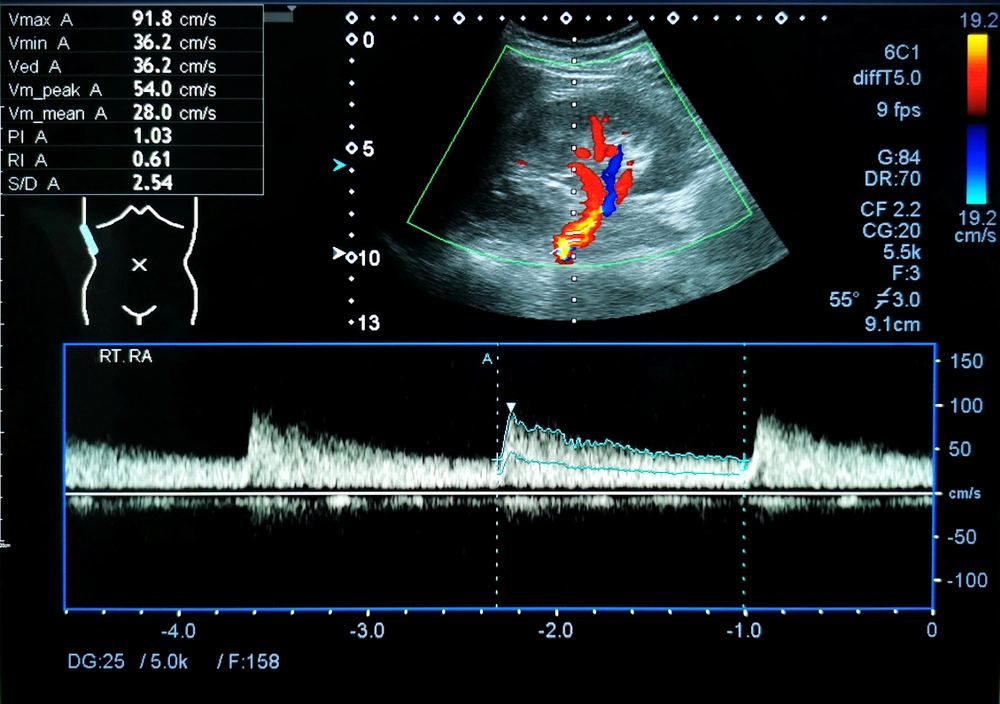
Ultrasound with Doppler: First-Line Modality
Ultrasound with Doppler is the primary imaging modality used in post-transplant surveillance due to its non-invasive nature, real-time assessment capabilities, and lack of ionizing radiation. It is particularly useful for evaluating renal perfusion, detecting vascular complications, and identifying parenchymal changes that may indicate rejection. Renal transplant Doppler ultrasound protocols assess blood flow in the renal artery, renal vein, and intrarenal vessels, helping clinicians determine whether the transplant is adequately perfused. A normal resistive index (RI) typically ranges from 0.6 to 0.8, signifying good vascular resistance. Any deviation from this range, such as an elevated RI, may indicate conditions like rejection, renal vein thrombosis, or external compression of the graft. Additionally, renal transplants Doppler ultrasound protocol findings such as loss of triphasic waveforms, turbulent flow, or increased velocity can suggest arterial stenosis or occlusion, necessitating further evaluation with advanced imaging.
- Purpose: Assess renal perfusion and detect vascular complications.
- Key Findings:
- Normal resistive index (RI) (0.6–0.8).
- Patent renal artery and vein with triphasic waveforms.
- No evidence of rejection-related changes (elevated RI, parenchymal swelling).
CT/MRI for Complications
While ultrasound serves as the first-line imaging modality, CT and MRI provide more detailed anatomical assessment when complications arise. CT is particularly effective for evaluating post-surgical hematomas, urinomas, lymphoceles, or vascular thrombosis, offering high-resolution images that guide clinical decision-making. It is often used in cases where ultrasound findings are inconclusive or when more precise localization of abnormalities is required. However, the use of iodinated contrast in CT scans is a concern for transplant patients with impaired renal function. In such cases, MRI becomes the preferred imaging option, especially for patients requiring contrast-free evaluation. MRI offers excellent soft tissue contrast and is particularly useful for detecting subtle parenchymal changes, assessing perfusion, and evaluating vascular structures with non-contrast techniques like MR angiography. Together, CT and MRI serve as valuable tools in diagnosing and managing post-transplant complications, ensuring optimal graft function and long-term transplant success. MRI becomes the preferred imaging option due to its contrast-free vascular assessment capabilities.
- CT angiography of kidneys: Evaluates post-surgical hematomas, urinomas, or vascular thrombosis.
- MR angiography of kidneys: Preferred for patients with renal insufficiency requiring contrast-free imaging.
Conclusion
Imaging plays a pivotal role in renal transplant procedures, from donor selection to recipient evaluation and post-transplant monitoring. Strict adherence to imaging protocols ensures accurate assessment, optimizes surgical planning, and enhances patient outcomes. Renal transplant ultrasound, CT angiography of kidneys, and renal transplant Doppler ultrasound protocols are crucial techniques for accurate assessment.
Looking ahead, emerging technologies such as AI-assisted imaging, automated vascular mapping, and contrast-free MRI techniques are set to revolutionize the field of renal transplant imaging. AI-driven tools can enhance the accuracy of renal vessel segmentation and predict potential complications, aiding radiologists in real-time decision-making. Additionally, advancements in non-contrast MRI will provide safer imaging alternatives for patients with renal impairment, further expanding the accessibility of preoperative imaging.
As these technologies continue to evolve, they will undoubtedly improve efficiency, reduce risks, and enhance renal transplant outcomes for both donors and recipients.
References
- NKF Statement: A Path Forward for Increasing Kidney Transplantation https://www.kidney.org/
- Vascular imaging in renal donors https://pmc.ncbi.nlm.nih.gov/
- Radiological Screening Methods in Deceased Organ Donation: An Overview of Guidelines Worldwide https://www.frontierspartnerships.org/
Disclaimer: The information provided on this website is intended to provide useful information to radiologic technologists. This information should not replace information provided by state, federal, or professional regulatory and authoritative bodies in the radiological technology industry. While Medical Professionals strives to always provide up-to-date and accurate information, laws, regulations, statutes, rules, and requirements may vary from one state to another and may change. Use of this information is entirely voluntary, and users should always refer to official regulatory bodies before acting on information. Users assume the entire risk as to the results of using the information provided, and in no event shall Medical Professionals be held liable for any direct, consequential, incidental or indirect damages suffered in the course of using the information provided. Medical Professionals hereby disclaims any responsibility for the consequences of any action(s) taken by any user as a result of using the information provided. Users hereby agree not to take action against, or seek to hold, or hold liable, Medical Professionals for the user’s use of the information provided.
