Rad Tech’s Role in Radiation Dose Management in Angiography

Radiation Dose Management and Safety in Angiography: The Crucial Role of Radiologic Technologists
When it comes to angiography, achieving the perfect image is a balancing act—like walking a tightrope between diagnostic clarity and radiation safety. This sophisticated imaging technique allows clinicians to visualize blood vessels with remarkable precision but also carries inherent risks associated with ionizing radiation. At the heart of managing these risks is the radiologic technologist, whose role in radiation dose management is pivotal in ensuring patient and staff safety. In this article, we will review the role of the radiologic technologist in managing radiation safety protocols during angiography procedures.
Radiologic Technologists: Guardians of Radiation Safety
Radiologic technologists are the frontline defenders in radiation dose management. They are responsible for optimizing exposure parameters to achieve diagnostic-quality images while minimizing radiation dose. This involves meticulous attention to technical settings such as kVp, mA, and exposure time, as well as the strategic use of dose-saving technologies like pulsed fluoroscopy and last image hold, both of which play a critical role in effective radiation dose management.
Key Methods for Dose Optimization:
- Pulsed Fluoroscopy: Instead of continuous radiation, pulsed fluoroscopy delivers radiation in quick bursts, significantly reducing the cumulative dose without compromising image quality. Adjusting the pulse rate to the lowest acceptable setting for the clinical task can dramatically decrease radiation exposure, contributing to efficient radiation dose management.
- Last Image Hold (LIH): This feature allows the last fluoroscopic image to remain displayed on the monitor without additional radiation exposure. Technologists should utilize LIH whenever possible to review anatomy and guide procedures, minimizing the need for repeated exposures.
- Optimizing Technical Parameters: Adjusting kVp (kilovolt peak) and mA (milliamperes) to the patient’s size and the diagnostic requirement is crucial. Using the lowest possible mA and appropriate kVp reduces the dose while maintaining image quality.
- Collimation: Narrowing the X-ray beam to the area of interest minimizes radiation scatter and reduces patient dose. Technologists should continuously adjust collimation throughout the procedure.
- Distance and Shielding: Maximizing the distance between the X-ray source and the patient, and between the patient and staff, reduces radiation intensity. Employing protective shields whenever feasible adds an extra layer of safety.

Ensuring Proper Use and Maintenance of Protective Wear
One of the technologist’s key responsibilities is to ensure that all personnel in the angiography suite are equipped with appropriate protective gear, including lead aprons, thyroid shields, and lead glasses. Proper fitting and correct usage of this equipment are critical to reducing occupational exposure.
Equally important is the regular inspection and maintenance of protective wear. Technologists must routinely check for signs of wear and tear, such as cracks or thinning in lead aprons, and ensure that defective equipment is promptly repaired or replaced. This proactive approach significantly contributes to a safer working environment.

General Guidelines for Inspection and Maintenance:
- Frequency of Inspection: Protective wear should be visually inspected before each use to identify any obvious damage. Additionally, a thorough inspection, including radiographic or fluoroscopic assessment, should be conducted at least annually, as recommended by radiation safety guidelines.
- How to Check: Begin with a visual inspection under good lighting, looking for tears, cracks, or creases, particularly along seams, folds, and areas of frequent bending. Follow this with a manual check by feeling for thin spots or irregularities in the material. For a more detailed evaluation, fluoroscopic screening can detect hidden cracks or defects that are not visible to the naked eye.
- Documentation: Maintain detailed records of all inspections, including the date, the condition of the equipment, and any corrective actions taken. This documentation ensures accountability and helps track the lifespan of protective gear.
- Storage Practices: Proper storage can prevent damage. Lead aprons should be hung on designated racks without folding to avoid creases, which can compromise their integrity over time.
Controlling Room Occupancy During Exposure
Radiologic technologists play a crucial role in managing the number of individuals present in the angiography room during radiation exposure. Only essential personnel should be in the room to minimize unnecessary exposure. The technologist ensures that non-essential staff and bystanders are either outside the room or positioned behind protective barriers, which is a critical practice for effective radiation dose management.
Table: Room Occupancy Guidelines During Angiography Procedures
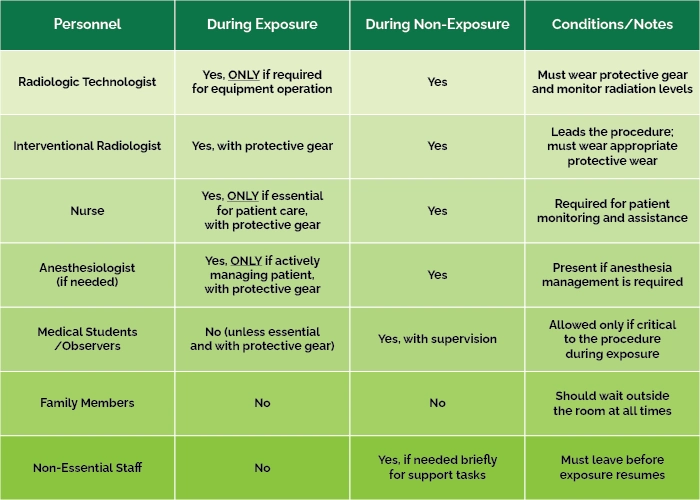
This structured approach ensures that only necessary personnel are exposed, thereby enhancing overall radiation safety and supporting comprehensive radiation dose management.
Managing Contrast Media and Patient Safety
While radiation dose management is a primary concern, technologists also play a vital role in the safe administration of contrast media. They are responsible for verifying that the contrast agent is appropriate for the patient’s condition and ensuring that the dose is tailored to the patient’s body habitus and clinical needs.
Pre-procedural screening is critical. Technologists must check for contraindications such as a history of allergic reactions to contrast agents or elevated creatinine levels, which could indicate impaired kidney function. This vigilance helps prevent adverse reactions and enhances overall patient safety.
Key Guidelines for Managing Contrast Media:
- Contrast Media Dose Considerations: Adjust the volume and concentration of contrast media based on the patient’s size, vascular condition, and type of angiographic study. Using lower doses can reduce both radiation exposure (as less imaging time may be required) and contrast-related risks, contributing to effective radiation dose management.
- Checking for Possible Allergies:
- Pre-Procedure Assessment: Obtain a thorough patient history focusing on previous reactions to contrast agents, known allergies (especially to iodine), and history of asthma or other allergic conditions.
- Premedication Protocols: For patients with a known allergy to contrast media, follow institutional protocols for premedication, which may include corticosteroids and antihistamines, to reduce the risk of adverse reactions.
- Emergency Preparedness: Ensure that emergency medications and equipment are readily available in case of an acute allergic reaction.

- Assessing Renal Function (Creatinine Levels):
- Baseline Evaluation: Check recent creatinine levels and calculate the estimated glomerular filtration rate (eGFR) to assess kidney function, particularly in patients with risk factors such as diabetes, hypertension, or a history of kidney disease.
- Risk Mitigation: For patients with elevated creatinine levels or reduced eGFR, consider alternative imaging modalities if feasible, use the lowest possible contrast dose, and ensure adequate hydration before and after the procedure to minimize the risk of contrast-induced nephropathy.
- Storage Practices: Proper storage can prevent damage. Lead aprons should be hung on designated racks without folding to avoid creases, which can compromise their integrity over time.
Pre-procedural screening is critical. Technologists must check for contraindications such as a history of allergic reactions to contrast agents or elevated creatinine levels, which could indicate impaired kidney function. This vigilance helps prevent adverse reactions and enhances overall patient safety.
Conclusion and Recommendations
In the dynamic environment of the angiography suite, radiologic technologists are much more than equipment operators. They are integral members of the healthcare team, balancing the need for high-quality diagnostic images with the imperative to minimize radiation exposure. Through careful dose management, diligent use of protective equipment, and vigilant patient care, technologists ensure that the dance between precision and protection is executed flawlessly, safeguarding both patients and medical staff.
As a final thought, it’s essential to recognize that this article serves as a general guide, highlighting critical areas of focus in angiography procedures. For specific protocols and detailed guidance, radiologic technologists should always refer to their hospital’s policies, state and federal regulations, and professional guidelines from organizations such as the American College of Radiology (ACR) and relevant radiation safety committees. Each institution may have unique procedures tailored to its operational environment, and staying up to date with these is vital.
Ultimately, a commitment to continuous learning, strict adherence to established safety standards, and effective collaboration with the healthcare team will ensure the highest level of care for both patients and staff in the angiography suite.
Disclaimer: The information provided on this website is intended to provide useful information to radiologic technologists. This information should not replace information provided by state, federal, or professional regulatory and authoritative bodies in the radiological technology industry. While Medical Professionals strives to always provide up-to-date and accurate information, laws, regulations, statutes, rules, and requirements may vary from one state to another and may change. Use of this information is entirely voluntary, and users should always refer to official regulatory bodies before acting on information. Users assume the entire risk as to the results of using the information provided, and in no event shall Medical Professionals be held liable for any direct, consequential, incidental or indirect damages suffered in the course of using the information provided. Medical Professionals hereby disclaims any responsibility for the consequences of any action(s) taken by any user as a result of using the information provided. Users hereby agree not to take action against, or seek to hold, or hold liable, Medical Professionals for the user’s use of the information provided.
