Patient Safety in Medical Imaging – Infection Control

Patient Safety in Medical Imaging – Infection Control


Introduction
The significance of basic infection control and the methods healthcare professionals can use to prevent disease transmission in clinical settings are crucial aspects of patient safety. The primary professional roles of radiographers and radiologists center on leveraging their skills to benefit patients while consistently ensuring patient safety. Numerous patient safety concerns in radiology must be addressed, with infection control being the focus of this article.
Reviewing common terms in epidemiology and infection control, and an overview of common pathogens in the medical imaging environment can help us remember why these practices are vital in our daily work. Let’s begin by examining the objectives to reinforce our understanding of infections.
Objectives
- Define terms associated with epidemiology and infection control
- Identify the most common pathogens found in the healthcare setting
- Describe the common transition routes in the spread of infection
- Explain infection control methods in medical imaging
Research from the onset of COVID-19 in the 2020 pandemic warranted policy development, including the methods adopted by healthcare workers to meet the needs of patients during this time. Healthcare-associated infections (HAIs) are caused by pathogenic microorganisms, which can be detected in the air, water, and surfaces. The modes of spread of HAIs include direct, indirect, and airborne contacts. The most prevalent HAIs that happen within healthcare institutions include respiratory infections, urinary tract infections, blood infections, and wound infections succeeding surgical procedures. As radiographers have direct contact with patients and other hosts, they are reported as being at an elevated risk of contracting and spreading infections.
Common Pathogens
Hospital-acquired infections are nosocomial-acquired infections. They are typically not present or might be incubating at the time of admission. These infections are usually acquired after hospitalization and manifest 48 hours after admission to the hospital. The infections are monitored closely by agencies including the National Healthcare Safety Network (NHSN), the National Institute of Health and Care Excellence (NICE), and the Centre for Disease Control and Prevention (CDC).
Methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas aeruginosa bacteria are the most common causes of pneumonia in patients. Early onset hospital-acquired pneumonia is usually seen less than 5 days after patient admission to the hospital and is usually caused by Streptococcus pneumonia. Late-onset pneumonia, seen more than 5 days after admission to a hospital, is commonly caused by microorganisms that are acquired in the hospital, such as MRSA, P. Aeruginosa, and other non-pseudomonal gram-negative bacteria.

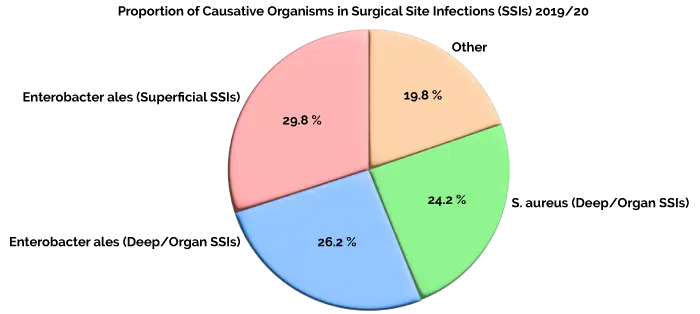
Surgical site infections (SSIs) have been shown to compose up to 20% of all healthcare-associated infections. At least 5% of patients who undergo a surgical procedure will develop a surgical site infection. A surgical site infection may range from a spontaneously limited wound discharge occurring within 7 to 10 days of an operation to a life-threatening postoperative complication, such as a sternal infection after open heart surgery. Enterobacter ales including Escherichia coli, Klebsiella, Salmonella, and Shigella continued to make up the largest proportion of causative organisms across all surgical categories in 2019/20 for both superficial SSIs (29.8%) and deep or organ/space (26.2%). However, S. aureus still contributes to a substantial proportion of deep or organ space SSIs (24.2%).
Sepsis is a clinical syndrome caused by the body’s immune and coagulation systems. They are activated by infections (bacteria, viruses, or fungi). Sepsis is one of the most common causes of death among hospitalized patients in the intensive care unit (ICU). The most common causes of sepsis in adults are pneumonia, bowel perforation, urinary tract infection, and severe skin infection. Group B streptococcus is the leading cause of both neonatal and maternal sepsis, though E. coli is an emerging threat. Both these pathogens have displayed considerable resistance to treatment and are considered priority pathogens for research and development of new antibiotics.
Clostridium difficile (c-diff) is now recognized as the leading cause of healthcare-associated infective diarrhea and is increasingly linked to community-acquired cases of colitis. C. diff bacteria are found in the digestive system of about 1 in every 30 healthy adults. Uncomplicated UTIs typically affect individuals who have no structural or neurological urinary tract abnormalities, typically affecting women, children, and elderly patients who are otherwise healthy. Complicated UTIs are usually associated with indwelling catheters, urinary tract abnormalities, immunosuppression, or exposure to antibiotics. The most common causative agent for both uncomplicated and complicated UTIs is uropathogenic E. coli (UPEC), accounting for almost 75% and 65% of all UTI cases, respectively. An acute UTI occurs in up to 50% of women and some estimates suggest that by the age of 24 years, thirty-three percent of females will have had at least one episode of cystitis.

Definitions
Epidemiology is the branch of medical science that investigates all the factors that determine the presence or absence of diseases and disorders. Epidemiological research helps us understand not only who has a disorder or disease but why and how it was brought to this individual or region. One of the earliest instances of modern epidemiology can be found during an 1854 cholera outbreak in London. Doctors believed the widespread illness must have been airborne, but Dr. John Snow, widely considered to be the father of epidemiology, employed a different kind of thinking. By carefully mapping the outbreak and analyzing those who were infected, Snow was able to link every cholera case to a single water pump at the intersection of Broad and Cambridge Streets (now Lexington Street) in London’s Soho neighborhood. The removal of the pump stopped the disease in its tracks—laying the basis of today’s epidemiological practices. This research helps us to understand how many people have a disease or disorder, if those numbers are changing, and how the disorder affects our society and our economy.
- Incidence: The number of new cases of a disease or disorder in a population over a specific time period
- Prevalence: The number of existing cases of a disease in a population at a given time
Contact tracing: In an attempt to stop the spread of disease and understand where it might go next, public health workers use contact tracing to determine the connections of an infected person. Currently, contact tracing is the process health departments use to collaborate with people who have been in close contact with someone with infections, such as COVID-19.

Transmission of infectious agents within a healthcare setting requires three elements: a source (or reservoir) of infectious agents, a susceptible host with a portal of entry receptive to the agent, and a mode of transmission for the agent. Transmission refers to the way pathogens are moved to the susceptible person. There are a few general ways that germs travel in healthcare settings – through contact (i.e., touching), sprays and splashes, inhalation, and sharps injuries (i.e., when someone is accidentally stuck with a used needle or sharp instrument). Pathogens that cause health care-associated infections (HAIs) are known to survive on surfaces and equipment in health care environments despite routine cleaning. As a result, the infection status of prior room occupants and roommates may play a role in HAI transmission. Within the hospital, healthcare workers (HCWs) are often exposed to infections. Any transmissible disease can occur in the hospital setting and may affect HCWs. HCWs are not only at risk of acquiring infections but also of being a source of infection to patients. Therefore, both the patient and the HCW need to be protected from contracting or transmitting hospital-acquired infections by using recommended infection control measures.
Infection Control: There are two tiers of recommended precautions to prevent the spread of infections in healthcare settings: Standard Precautions and Transmission-Based Precautions. They are based on a risk assessment and make use of common-sense practices and personal protective equipment that protect healthcare providers from infection and prevent the spread of infection from patient to patient.

Standard Precautions should be used for all patient care. They are based on a risk assessment and make use of common-sense practices and personal protective equipment use that protect healthcare providers from infection and prevent the spread of infection from patient to patient.
Transmission-based precautions are the second tier of basic infection control and should be used in addition to standard precautions for patients who may be infected or colonized with certain infectious agents for which additional precautions are needed to prevent infection transmission.
Infection prevention and control is the cornerstone of a resilient healthcare system and protects health workers, patients, and the surrounding community. The COVID-19 pandemic has demonstrated that many health systems worldwide are challenged by daily needs for healthcare safety and are unprepared to respond to the emergence of a new infectious disease.
Summary
Issues identified from my literature review resulted in seven sets of recommendations to help control the spread of infections in the healthcare setting: hand hygiene, personal hygiene, personal protective equipment (PPE) and the use of appropriate equipment, safe handling of sharps and sharp containers, decontamination, and cleaning, housekeeping and routine infection control practices. Policies put in place for those patients on a COVID unit, or any patient suspected of having a highly contagious disease should always be followed. Patient safety, especially infection control, is one of the most important roles of all healthcare professionals.
References
- Patient Safety in Medical Imaging https://pubmed.gov/
- What Is Epidemiology? | Columbia Public Health, https://www.publichealth.edu/
- https://inivos.com/
- Flores-Mireles, A., Walker, J., Caparon, M. et al. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 13, 269–284 (2015). https://doi.org/
- COVID-19 Contact Tracing Communication Toolkit for Health, https://www.cdc.gov/
- Transmission-Based Precautions | Basics | Infection. https://www.cdc.gov/
- https://www.ncbi.gov/
- National Health Services Professionals Handbook, 2010, Standard infection control precautions. Clinical governance, National Health Service, London.
- https://www.nidcd.gov/
- https://www.publichealth.edu/
- https://www.publichealth.edu/
- https://www.pubmed.gov/
- https://www.cdc.gov/
- https://www.cdc.gov/
- https://www.cdc.gov/
- https://www.cdc.gov/
