Radiation Therapists’ Role in the CT Simulation Room

Radiation Therapists’ Role in the CT Simulation Room – Radiation Therapy Simulation

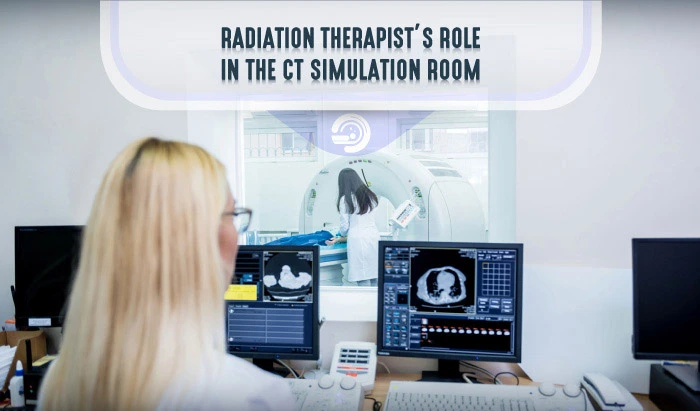
Radiation therapists play multiple, important roles in the treatment of patients with cancer. As part of the oncology teams that treat patients with cancer, radiation therapists operate machines that deliver concentrated radiation therapy to the region of a patient’s tumor. Before radiation treatment begins, radiation therapy teams carefully plan treatment in a process called radiation simulation. Radiation therapists have many duties and responsibilities in radiation therapy simulation. This guide aims to assist radiation therapists with their clinical routines in CT simulation, including scanner preparation, verification of the necessary equipment, case and patient preparation, setup and immobilization, CT simulation, patient orientation, and documentation.
Scanner Preparation in CT Simulation
Before any operation, you must prepare the simulation scanner. This procedure differs depending on the department’s protocols, the machine manufacturer, and the test phantom used.
- Warm-up the X-ray tube
- After starting the CT, begin a predefined protocol in terms of kilovoltage, milliamperage, and other acquisition parameters
- Then, carry out tests of the quality of the images produced and their geometric characteristics
Verification of the Necessary Equipment in CT Simulation
The CT simulation room must be well equipped with the necessary material for nursing care, immobilization, and localization. It is the responsibility of the radiation therapist to make sure everything is in order. The required equipment for nursing care, immobilization, and localization are listed in the collapsibles below. Click the menu headings to read more.
Nursing Care Equipment
You must check the availability of the necessary equipment for nursing care, among which we mention the antiseptic, gloves, gauze, face masks, oxygen mask, and the IV kit.
Immobilization Equipment
In order to have a reproducible position during treatment, the patient must be immobilized with devices specific to the localization to be treated. The same accessories available in the radiation simulation room must be also available in the treatment room.
- A water bath: containing water heated to about 70 degrees Celsius, where the thermoplastic mask is soaked to become malleable
- A personalized thermoplastic mask that will adhere to the shape of the patient’s face
- Adhesive tape, which will be stuck on the made-up mask and on which the reference points will be marked
- A flat or angled support, on which the patient will lie down, to horizontalize the spine and lower the shoulders as much as possible with the arm-rests
- Head-rests or foam cushions to slide under the patient’s neck; these are available in several shapes and thicknesses and must be chosen depending on the desired neck extension and the patient’s morphology and comfort
- A mouthpiece to reproduce the opening of the mouth and push the tongue down and back to allow better protection

For the irradiation of the thoracic region, wing support is required to keep the arms away from the X-ray beam.
- An inclined support to slide under the patient’s chest to horizontalize the chest wall; there are different angulations to suit patients’ individual morphologies
- And two pairs of elbow and wrist rests, right and left, to hold the arms away from the treatment field


- Vaginal and rectal markers; can be useful for better visualization of the limits
- Knee-fix and feet-fix, for good immobilization of the legs and feet
- A pillow to be positioned under the patient’s head for comfort
- Polystyrene mattresses, which conform to the exact shape of the patient
- Abdominal compressions, used mainly to limit the movement of the patient’s abdomen caused by breathing; very useful for certain SBRT treatments
Sometimes, for the treatment of colon cancer, radiation oncologists prefer the use of the prone support, called a belly board.


- Markers for drawing on the skin and an A graduated ruler
- Lead wire to identify scars and lymph nodes and lead balls to be fixed on the reference points
- Ink and a small needle, or a tattoo machine
- Contrast media for tumors of the esophagus, stomach, and rectum
Case Preparation in CT Simulation
After verifying that all the necessary equipment is available in the radiation therapy simulation room, you should prepare the patient’s medical file. The file must contain previous radiology exams, reports of surgical procedures, histological and biological analyses, as well as the decided treatment plan, namely, the target volume, the total dose, the dose fractionation, and the treatment technique. Register the patient by entering identification details, such as their first and last name, their unique medical identification number, and the localization to be imaged. Then set up the appropriate immobilization devices on the scanner table. If it is a head or neck scanner, preheat the water bath.
Patient Preparation in CT Simulation
- Call the patient and guide them to the locker room, observing the safety measures of ensuring the correct identification of the patient, the presence of parental assistance for children and the elderly, screening for the risk of pregnancy, and asking the patient to sign the consent form
- Prepare the patient psychologically by explaining to them the process of the examination, the usefulness of the CT simulation, the purpose and use of indelible skin marks, the need for them to remain absolutely immobile during the radiation simulation and treatment
- Be sure to mention that the procedure is painless. Reassure the patient that they will be monitored at all times, and that they will be able to communicate with you constantly
- For pelvic irradiation, such as for the prostate and the uterus, home preparation is requested and explained by the doctor during consultation. It is imperative that you evaluate the patient’s preparation by questioning, knowing that in most cases, the rectum must be empty and the bladder must be full
- Finally, ask the patient to undress and put on a gown to proceed to the next step
Setup and Immobilization
Once the patient is ready, help them to settle down on the table in as stable and comfortable a position as possible, while taking into account their physical capacities and respecting the indications of the treatment plan. In most cases, the patient will be placed in a supine position. In some cases, the patient will be placed in a prone position, as for irradiation of the spinal cord or lumbar spine. Very specific cases require that the patient be placed in a lateral position. The patient must be properly aligned with the appropriate immobilization devices.


CT Simulation
- Carefully move the scanner’s table vertically and horizontally towards the gantry
- Acquire the scout view
- Ensure the perfect alignment of the patient. Reposition the patient if necessary, and draw the midline
- The radiation simulation will be performed in collaboration with the radiation oncologist
- The physician will identify the target at which the radiation will be directed and the organs to be protected
- You must define the limits of the slices
- Mark on the skin or on the immobilization device the three reference points represented by the intersection of the lasers in front and on both sides
- Fix the lead balls on these marks
- Acquire the CT
- You can also take a photo of an unusual positioning, which will help to reproduce the position during treatment
- Once the scanner is done, return the table to its initial position. Remove the lead wires and balls and tattoo the reference points with very fine disposable needles and ink
Patient Orientation
Once the radiation simulation is done, you must explain the hygiene rules the patient must follow. Mention that they should not apply anything to their skin: no perfume, deodorant, or shower gel. Explain to the patient that they should use Marseille soap to wash the irradiated area and that they should wear cotton clothing and avoid exposure to sunlight. Also, highlight that the position adopted during the radiation therapy simulation is that which the patient will have to reproduce at each treatment session and that the immobilization devices will be the same. For pelvic irradiation, it should be emphasized that home preparation is necessary for all treatment sessions. Then, refer the patient to reception to get an identification photo and an appointment card for treatment sessions and follow-up consultations.

Documentation
- The patient’s medical and social information
- The therapeutic indication: the total dose, the number of sessions, and the dose per fraction, e.g., 70 Gy for 35 sessions 5 times a week or 2 Gy per session
- The immobilization devices used, including the necessary details, such as the degree of inclination of the inclined board for the breast
- The positioning instructions
These can be documented on paper, on special computer software, or both.
Then, you must export the CT images to the treatment planning system located in the physics unit and send them the patient file.
Final Thoughts on the Role of Radiation Therapists’ in Radiation Therapy Simulation
In addition to ensuring the preparation of the equipment, the calibration of the machines, and delivering targeted radiation therapy to the region(s) affected by patient’s cancer, radiation therapists play another critical role in the CT simulation room: they work to provide patients with emotional support and comfort during the radiation simulation and treatment. Although radiation therapists have a technical job, it is crucial that they remain aware of their role in providing patient care and take appropriate steps to ensure that they support patients in feeling comfortable during their radiation therapy.