Dedicated CT Imaging of the Breast



This article is part of our series on computed tomography (CT). Here, we address breast anatomy, physiology, and pathologies, as well as the history of dedicated breast CT imaging systems. This article also includes an overview of current research in breast CT scan, cone beam breast CT and a comparison of breast CT to standard mammography.
Breast Anatomy and Physiology
- Glandular tissue includes the breast lobes and breast ducts
- Fibrous, or supportive or connective, tissue is the same tissue that ligaments and scar tissue are made of
- Fatty tissue fills in the spaces between glandular and fibrous tissue and largely determines breast size
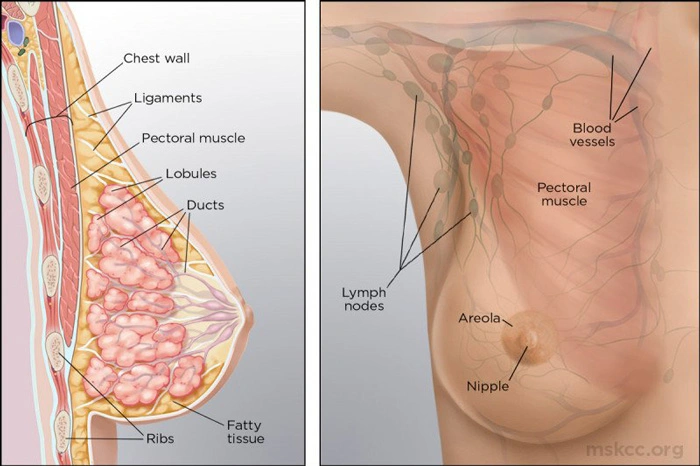
Source: https://www.mskcc.org/
Embedded in the breast’s fatty and fibrous tissue are 15-20 glands referred to as lobes. Each lobe has many smaller milk-producing lobules, or sacs. These lobules are arranged in clusters that resemble bunches of grapes.
The thin tubes that carry the milk to the nipple, which is in the middle of the darkened areola, are known as ducts. Breast cancers can form in both the ducts and the lobes.
Dedicated Breast CT Research
Several research groups in the United States and in European Union have been developing CT systems with dedicated digital detector technology to image the uncompressed breast since 2001. While overcoming some of the limitations of mammography, BCT maintains a level of radiation dose to the radiosensitive glandular tissue similar to that of two-view mammography for equal breast size and composition.
Breast CT is a cone beam CT system in which the woman lies prone on the table, with the single breast to be imaged hanging pendant through that hole. No breast compression is used.
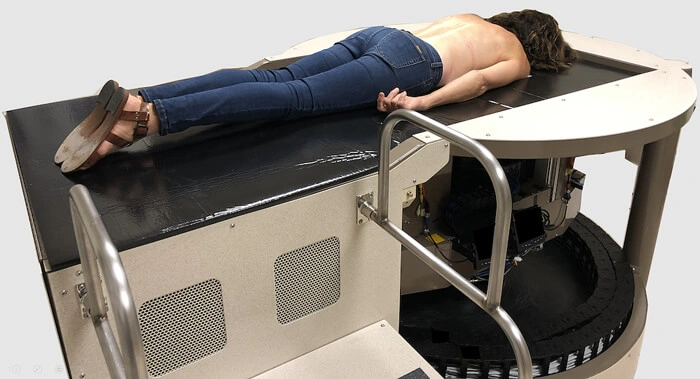
Source: https://health.ucdavis.edu/
During a ten second breath-hold, the cone beam CT apparatus below the table scans the breast in one rotation. This provides all the necessary data to reconstruct the full 3D image data set from that breast.
In their Boone lab, the University of California, Davis has studied the potential of dedicated CT for breast imaging for the past twenty years. During this time, four CT systems for the braest have been designed, fabricated, and tested. The cone beam CT apparatus, primarily an X-ray tube and a flat panel detector, rotates around the breast, producing hundreds of low-dose projection images of the breast.
The reconstructed full data set produces high-resolution (150 µm voxels) images of the breast in three dimensions.
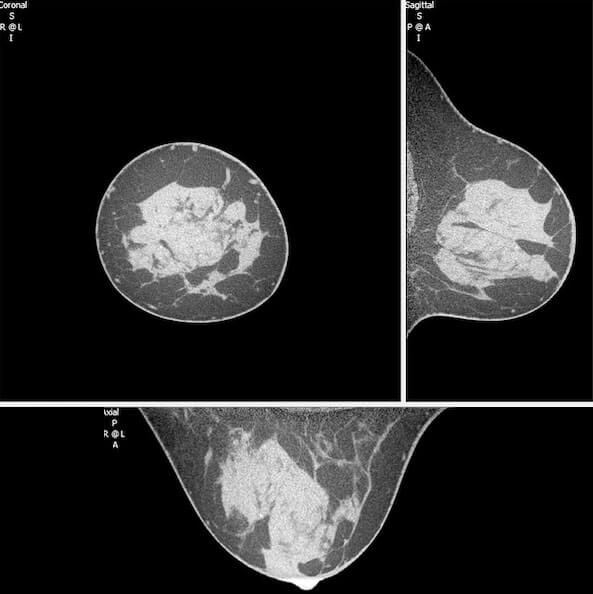
Source: https://health.ucdavis.edu/
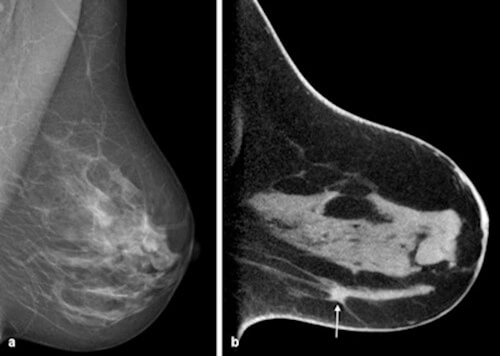
The projection images are reconstructed to produce a fully three-dimensional high-resolution image data set of the breast, as shown in Figure 3. It is important to note that this is a true 3D depiction of the breast, something that breast tomosynthesis is not capable of producing due to its limited angle characteristics. Using the CT systems in the Boone lab, about 600 patients have been imaged with both non-contrast and contrast agents. Summation artifacts and other abnormalities associated with 2D mammography are overcome because of the true 3D nature of these image data sets. Since the radiologist can view CT sections of the breast, this eliminates the superimposition of the tissue, making it more beneficial for evaluating dense breasts than 2D mammography.
Dedicated breast CT shows promise as an adjunct to mammography—with the added benefit of not requiring breast compression, according to a study conducted at Beth Israel Deaconess Medical Center. This study compared the clinical performance of breast CT with that of 2D standard-view screening mammography and 2D diagnostic mammography to evaluate its role in diagnostic breast imaging.
All 235 cases were compared and included screening mammography, diagnostic mammography, and dedicated CT images. A total of eighteen radiologists were used in interpreting the cases over the course of three sessions: breast CT alone, breast CT plus screening mammography, and diagnostic mammography alone. They tracked sensitivity, specificity, and area under the receiver operator characteristics (ROC) curve. Of the 235 cases, 52 were negative, 104 were benign, and 79 were malignant.
The study found that the combination of dedicated breast CT plus screening mammography had significantly higher sensitivity than diagnostic mammography and dedicated breast CT alone. This result suggests that dedicated CT for diagnostic imaging is most effective as an adjunct to the standard view mammography.
Source: https://www.auntminnieeurope.com/user/images/content_images/sup_cto/2016_05_05_11_02_28_712_2016_05_06_DRK2-fig2.jpg
A scanner developed at the University of Rochester uses a pulsed X-ray source and a 10-second acquisition. A total of 300 views are acquired at 30 frames per second. This scanner operates at a maximum of 49 kVp and uses a digital mammography X-ray tube designed with a tungsten anode. A pulsed X-ray tube design improves spatial resolution with a short duration (~8 ms) of each X-ray pulse essentially freezing the rotational motion of the gantry. The 10-second scan time should also be acceptable by women who undergo this breath-hold examination.
In 2019, a group of Swiss researchers conducted a feasibility study with a new breast CT scanner. This study showed that the system used produced high-quality images at low radiation dose. The combination could mean that breast CT scan could be ready for cancer screening. A team from the University of Zurich in Switzerland believes that breast CT has the potential to further improve breast lesion detection and characterization compared with mammography and digital breast tomosynthesis (DBT), particularly because it does not require breast compression. The photon-counting detector technology reduces the radiation dose to levels comparable to those of a conventional mammogram.
Leader of the study, Dr. Nicole Berger, “Previous studies investigating the use of cone beam breast CT in comparison to mammography reported higher radiation doses, especially when referring to a screening setting… More recently, new strategies have strongly increased the dose efficiency due to the use of novel photon-counting detector technology, resulting in dose levels for breast CT comparable to those of screening mammography or lower.” Another benefit is that it can be used with contrast. Until recently, the resolution of breast CT did not reach high enough resolution to visualize microcalcifications, which the new dedicated systems can provide.
Dedicated Breast CT Made Formally Accessible
In June of 2020, the American Medical Association (AMA) assigned 6 new Category III CPT codes for the FDA PMA cleared dedicated breast CT imaging procedure, marking the formal introduction of access to DBCT on January 1, 2021.
Recap
Dedicated breast CT is an imaging device of the breast that allows for a full 360-degree CT scan of the breast without compression. DBCT is currently under clinical investigation for patients who have suspicious findings from screening or diagnostic mammography. Initial studies demonstrate that this technology can help resolve the issue of overlapping tissue that could possibly be obscuring breast cancer and may provide physiologic information when intravenous contrast is used. In addition, this technology may provide more flexibility since it has faster scanner times and possibly more availability than MRI.
If you enjoyed this article on CT imaging of the breast, and are interested in learning more about CT, we recommend our CT Essentials and CT Advanced courses for your continuing education credits.
References
- https://www.mskcc.org/
- https://www.auntminnie.com/
- https://health.ucdavis.edu/
- Chen Z, Ning R. Why should breast tumor detection go three dimensional? Phys Med Biol. 2003 Jul;48(14):2217–2228. [PubMed]
- Lindfors, K. K., Boone, J. M., Newell, M. S., & D’Orsi, C. J. (2010). Dedicated breast computed tomography: the optimal cross-sectional imaging solution?. Radiologic clinics of North America, 48(5), 1043–1054. https://www.ncbi.nlm.nih.gov/
- Berger, Nicole MD; Marcon, Magda MD; Frauenfelder, Thomas MD; Boss, Andreas MD, PhD Dedicated Spiral Breast Computed Tomography With a Single Photon-Counting Detector, Investigative Radiology: February 2020 – Volume 55 – Issue 2 – p 68-72 doi: 10.1097/RLI.0000000000000609. https://journals.lww.com/
- http://koninghealth.com/
- https://www.ncbi.nlm.nih.gov/
- https://www.auntminnieeurope.com/
- https://healthmanagement.org/